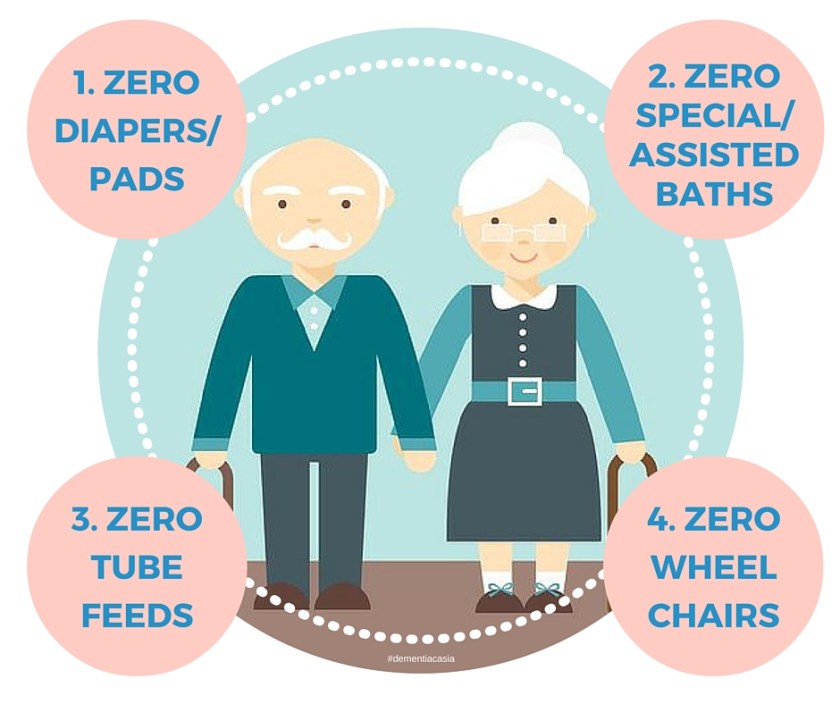
This is pretty amazing, a models of care from an organisation providing care in Japan. This is just incredible, it’s just so simple and functional.
At first glance, it looks confusing, like what? 4 big zeros? Zero wheelchairs? What does that mean? That the organisation don’t provide wheelchairs?

image from http://www.sompocare-next.jp/
4 zero is a really outstanding care philosophy, to ensure that the organisation work towards the physiological and mental health of the resident to ensure that their independence, dignity and autonomy is maintained as long as possible. So much so that until the end of days they will never have to live with diapers, assisted baths, tube feeding or wheelchairs.
1. Zero Diapers/pads
2. Zero Special baths
3. Zero Tube feeds
4. Zero Wheelchairs
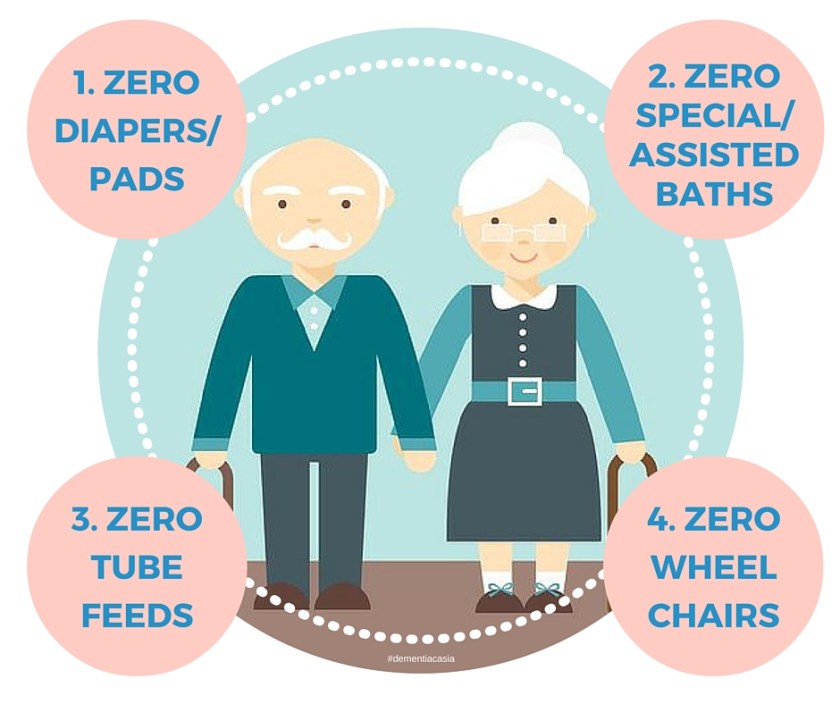
That really sums up the care that we need to provide to ensure that the people with dementia have a great quality of life. Too often we take it for granted that it’s okay for people to wear diapers/pads, to have assisted baths, to be on feed tubes and to grow old is to literally lose your mobility. Be it a home care service, residential aged care, or in acute care, that’s what we all should be aiming to help everyone live better. To ensure that people living with dementia can live healthy, respected and meaningful lives without the added pain, humiliation and anguish that we so flippantly systematically introduce into their lives.
Residents have told me that they are uncomfortable, humiliating, and some have even felt the need to become reclusive, as they are conscious that their pads or diapers may smell. This is awful for a person’s well-being. Living with dementia, it’s stressful enough to ensure that each day is lived to it’s fullest, to remember to do the things that they need to do. On top of that having to wear, change and walk around with a diaper or pad, really is one of the last things anyone really needs. Zero Diapers/Pads!

As a child, can you remember getting your body scrubbed and being twirled around to be mopped up in the shower. Like a military exercise, the shower never comes on when you want it and it’s always too hot or too cold. Think of the dances that you did and the anxiety it brings trying to avoid that first blast of water. The pelting of water smacking into your face when you least expected it. Lots of scrubbing and before you know it, it’s all done and you are bundled out faster a bag of groceries at the supermarket at lunch time.
Some people rally appreciated their showers, they sing in the shower, play with the foam in their hair in the shower, and just sometimes after a long day which feels like the end of the world, they may just stand in the shower with the water streaming down on me in silence. Just listening to the sound of the water, enjoying the calming warmth in serenity, it’s much needed especially after a rough day.
Having assisted baths are just not the same, and for anyone who has showered a resident. Residents have mentioned that they don’t care anymore and for some it is frustrating and they get annoyed especially if they get a different person helping them with their shower that they may not be familiar with, and rightly so. Imagine having a stranger seeing you naked or scrubbing you, or standing in the room watching you while you try and enjoy a warm shower. We should try and help people to maintain their independence and mobility as long as we possibly can, so that for everyone who enjoys a nice hot shower by themselves in private, they can keep rocking on. Zero Special/Assisted Baths!

Imagine never being able to eat. Food is the breath of life, from the moment of birth we taste the sweetest of milk, we lick the salt off the palm of our sweaty little hands and as we grow, continue to enjoy the luxurious experience of having a meal. We open our auditory perception to the vibrators around us, to the sound of chewing in our mouths, the crackle and pops, the slurping, chomping of meat and vegetables, the crunching of chips. We open our senses to a world of gustatory perception, from the sweetness of honey to the heat of the beloved bird’s eye chillis from Southeast Asia. Our 5000 taste buds activating their 100 taste receptor cells, kicking themselves into action, working hard to make each meal an adventure (Siverthorn 2007). When the odorant molecules creep towards us and bind themselves to our olfactory receptors, we can’t help but take in the information that these little molecules have given us and up the glomerulus, the information is sent, right into our olfactory bulb that helps us make sense of the delight close by. They say we eat with our eyes, and watching chefs like Jamie Oliver put together a feast before us, some say it’s almost as good as having the meal in itself. Let’s not even talk about the tactioception, the spring of a baked muffin out of the oven or themoception, the cold of a vanilla ice cream, or the warmth of Ramen on a winter’s afternoon.
Kuraoka & Nakayama (2014) stated that common causes of issues that might require percutaneous endoscopic gastrostomy (PEG) where a tube runs pass the mouth and through the adomon to deliver contents the stomache include;
- inability to independently have their meals as a result of cognitive deterioration
- loss of interest/appetite in having their meals as a result of depression or poor mental health
- damage to nerves and muscles required for the eating and swallowing in the event of stroke
Research (Taylor et al 1992), found that up to 70% of people with PEG will encounter complications ranging from minor to severe with survival probibility of 1.5 years to 4 years after referrel. Increased risk of death was also stated in the study and it was stated that individuals with people with low risk of survival will not benefit from having a PEG. A multitude of ethical issues that arise from PEG includes the stress and frustration that caregivers feel to have to make decisions regarding their loved ones being on PEG and most of these decision-making procession may only range for a few minutes, forcing caregivers to make an on the spot decision regarding this critical issue (Kuraoka & Nakayama 2014).
We should do our best to keep older adults, happy, healthy and independent and not flippantly take the important issues for granted and have people live with PEG feeding tubes/Nasal Gastric (NG) tubes. Zero Tube Feeds!

The last of all is a big issue and a lot of people grapple with nurses and caregivers alike. We are all afraid of our loved ones and residents falling, in Asia we are also attuned to over caring and being time poor it’s a lot easier for us to do things for others then to allow them to do it themselves with our assistance. We pride efficiency and timeliness at the cost of the independence for others. This however is not fully attributed to staff, Residents, families and clients have to be aware of these issues as well. They have to be aware of the issues that are tied to muscle atropher or disuse atrophy which occurs from loss of physical activity. It’s not uncommon to see a person after recovering from a fall, filled with intense anxiety and grappled with fear that they literally wake up, sit in a wheel chair and never find the strength to be mobile again. Some nursing staff may also have encountered residents who on top of not wanting to walk, insist on being pushed around in a wheelchair. Residents feel that they pay for their care and therefore they should be wheeled everywhere and should not lose out, as caregivers and families, do they realise that the emphasis on the dollar is impacting their cognitive and physical health resulting in their loss of movement?
Just the basic movement of walking, in the part to the bus shelter, getting up to grab a drink result in the activation of different muscle synergies and motor corticol regions in our brain. Each movement that we take for granted and carry out with ease sets off a blaze of neurons. Imagine walking in the garden or a park, feeling the sun on your face or the breeze, or the heat and humidity working up a sweat. We are surrounded by a constant ball of experiences, though little they make up a whole of how we conprehend and understand our bodies, mind and the environment around us. The simple things in life are lessons in itself. We know (Ahlskog 2011) that physical exercise is a critial cost-effective preventative element against dementia and brain aging, so why are organisations strapping their clients down and paying for programmes which may not have adequate evidence base in the preventative treatment of dementia and brain ageing?
We should be working towards enhancing, enabling and empowering people to be healthy and fit, to help them maintain their independence, autonomy and mobility in an inclusive environment. Zero Wheelchairs!
We have the obligations to provide good care for the people around us, to maintain a sense of harmony and homeostatis to keep our inclusive and complex society moving. Putting the needs of fulfilling black and white key performance indicators that provide quantitative information without any qualitative outcome for the people we are meant to care for is no outcome at all. What does it mean to give a part of ourselves and our time to pursure the more important and meaningful things in life and not just keeping up the numbers. Unlike the West, we were brought up with values that put the needs of society before our own, and we need to remember that and not pursue our own needs at all cost for our own brighter future at the risk of poorer health outcome for others.
References:
Ahlskog JE, Geda YE, Graff-Radford NR, Petersen RC. Physical exercise as a
preventive or disease-modifying treatment of dementia and brain aging. Mayo Clin
Proc. 2011 Sep;86(9):876-84.
de March, Claire A.; Ryu, SangEun; Sicard, Gilles; Moon, Cheil; Golebiowski, Jérôme (September 2015). “Structure–odour relationships reviewed in the postgenomic era”. Flavour and Fragrance Journal 30 (5): 342–361
Kuraoka, Y. & Nakayama, K., 2014. A decision aid regarding long-term tube feeding targeting substitute decision makers for cognitively impaired older persons in Japan: A small-scale before-and-after study. BMC geriatrics, 14(1), p.16. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24495735.
Rana M, Yani MS, Asavasopon S, Fisher BE, Kutch JJ. Brain Connectivity
Associated with Muscle Synergies in Humans. J Neurosci. 2015 Nov
4;35(44):14708-16.
Silverthorn, D. U. (2007). Human physiology: An integrated approach. San Francisco: Pearson/Benjamin Cummings.
Taylor CA, Larson DE, Ballard DJ, Bergstrom LR, Silverstein MD, Zinsmeister
AR, DiMagno EP. Predictors of outcome after percutaneous endoscopic gastrostomy:
a community-based study. Mayo Clin Proc. 1992 Nov;67(11):1042-9.
Other sources: 私たちの特長 | SOMPOケアネクストの有料老人ホーム・介護施設
Disclaimer: Just to be clear the blogger does not work or receive any funding from the company or organization in this article.












 1 in 10 Singaporeans over 60 have dementia. This number is set to rise quickly. Are we prepared for the onslaught? Justin Bratton experiences what life is like when warped by dementia. He heads to Japan to find out how the entire country is being mobilized to create a dementia friendly nation.
1 in 10 Singaporeans over 60 have dementia. This number is set to rise quickly. Are we prepared for the onslaught? Justin Bratton experiences what life is like when warped by dementia. He heads to Japan to find out how the entire country is being mobilized to create a dementia friendly nation.


